Osteoarthritis: Vitamin D Eases Movement and Fights Pain in Obese People
Osteoarthritis and obesity: vitamin D helps movement and reduces pain
Adequate vitamin D levels can improve movement and reduce joint pain in obese individuals affected by arthritis. The benefits of vitamin D could be due both to its ability to protect bones and to reduce inflammation.
This is explained by the results of a study conducted by researchers at the University of Florida (USA) and published in The Clinical Journal of Pain.
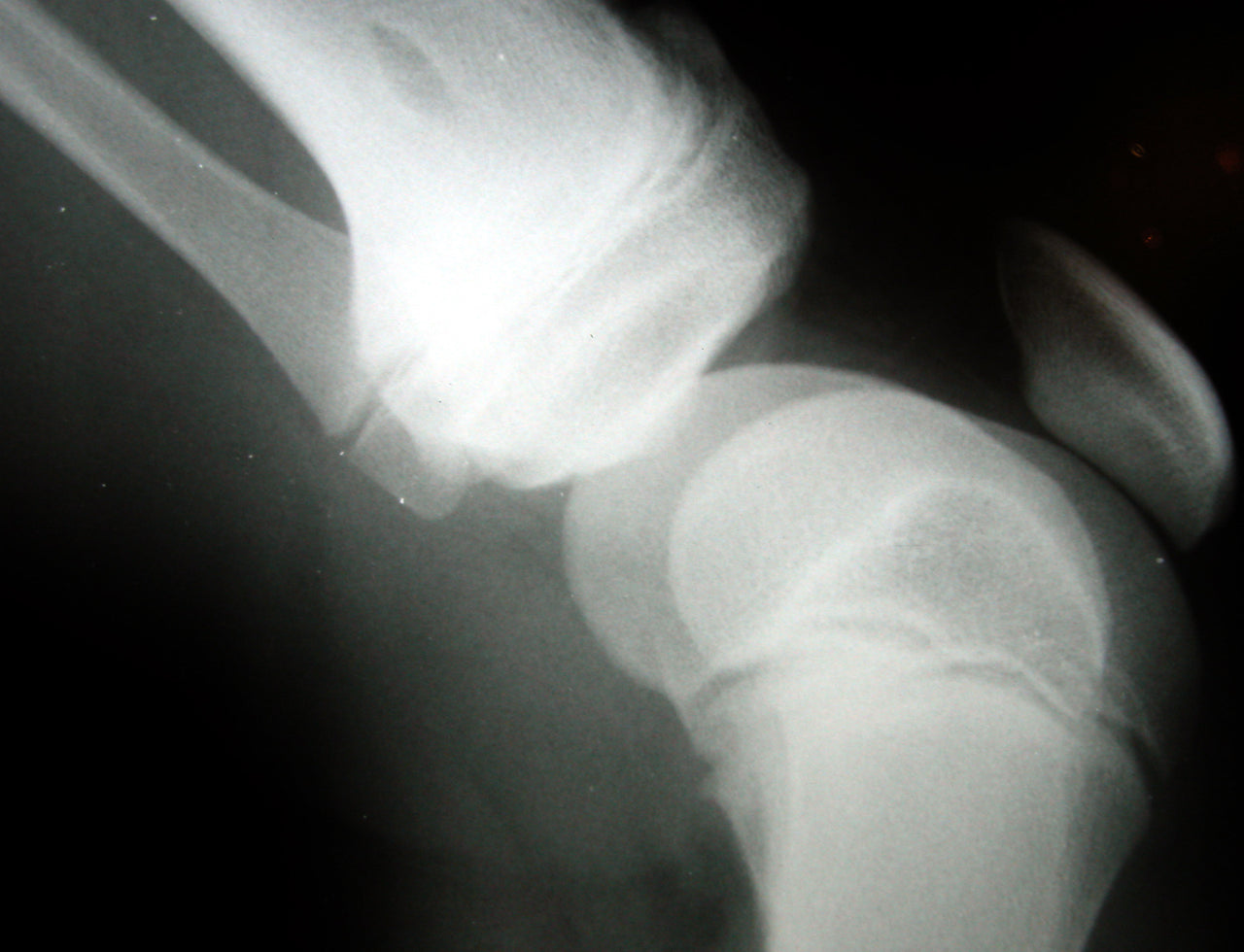
Osteoarthritis: a very common condition
Arthritis is a group of different conditions that share the characteristic of causing inflammation at the joint level, swelling, stiffness, and pain that lead to loss of joint function. The prevalence of knee arthritis is increasing with the aging population and is worsened by the growing number of obese and elderly people. Several studies in recent years have suggested that vitamin D deficiency in adults can worsen osteopenia, osteoporosis, muscle weakness, fractures, autoimmune diseases, infectious diseases, and cardiovascular diseases. Low vitamin D levels measured in serum as 25-hydroxyvitamin D (25(OH)D), in elderly and obese people, are associated with several health conditions including chronic pain.
Is there a relationship between vitamin D and osteoarthritis pain?
Dr. Glover, who led the study, and his colleagues collected and analyzed data from 256 people with an average age of 57 years. Participants reported knee osteoarthritis pain and underwent a lower limb functional performance test. Vitamin D levels were obtained by analyzing blood samples from each subject. Results showed that obese people with adequate vitamin D levels had less knee pain compared to obese individuals with vitamin D deficiency. Moreover, some motor performances, such as standing up from a seated position, appeared significantly better in those with higher blood vitamin D concentrations.
A relationship still to be explained
According to the authors, the study shows a relationship, but the potential mechanism explaining the association between vitamin D levels and improved function is not completely understood. It could be due to the anti-inflammatory action of vitamin D and its ability to maintain proper calcium and phosphate levels in the bones. Dr. Glover also emphasized that pain caused by osteoarthritis could limit physical activity, including outdoor activities, favoring further vitamin D deficiency (as sunlight stimulates its synthesis) and increasing obesity.
Source: T.L. Glover, B.R. Goodin, C.D. King, et al. “A Cross-Sectional Examination of Vitamin D, Obesity, and Measures of Pain and Function in Middle-Aged and Older Adults with Knee Osteoarthritis” The Clinical Journal of Pain. doi: 10.1097/AJP.0000000000000210





